 Cancer diagnosis and accurate selection of an appropriate treatment are an important result of a histologist’s work. Traditionally, cancer treatments have primarily included chemotherapy and radiation, but the last few decades have seen an increased focus on immunotherapies, treatments that utilize the patient’s own immune system to fight the cancer cells.
Cancer diagnosis and accurate selection of an appropriate treatment are an important result of a histologist’s work. Traditionally, cancer treatments have primarily included chemotherapy and radiation, but the last few decades have seen an increased focus on immunotherapies, treatments that utilize the patient’s own immune system to fight the cancer cells.
Research into immune cells as they relate to cancer dates back to the early 1960’s with initial studies proving the ability of immune cells to protect mice from cancer and the identification of the origin of immune cells, such as T-cells. By the 1990’s researchers began developing the chimeric antigen receptor (CAR) which would be used in CAR-T cell therapy, which after much refinement, reached clinical trials in 2012.
Immunotherapy uses something called adoptive cell transfer (ACT). This is the process of utilizing laboratory techniques to improve or expand the patient’s immune cells and return them to the body to fight the cancer. There are several different types of ACT, which include:
- Tumor-Infiltrating Lymphocyte (TIL) Therapy
- Engineered T Cell Receptor (TCR) Therapy
- Chimeric Antigen Receptor (CAR) T Cell Therapy
- Natural Killer (NK) Cell Therapy
Tumor Infiltrating Lymphocyte Therapy: In this therapy, the patient’s T-Cells have recognized the tumor, but there is not enough of them and they cannot sustain the level of activity needed to get the job done. TIL activates the T-Cells and makes more of them, to be infused into the patient.
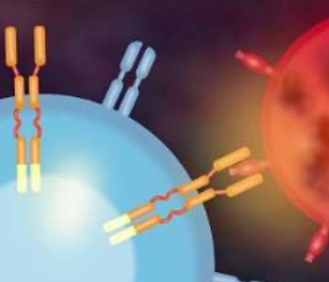
Engineered TCR Therapy and Chimeric Antigen Receptor Therapy: Engineered T-Cell Receptor (TCR) and Chimeric Antigen Receptor (CAR) therapies are very similar, in that they both involve attaching receptors to the cells so they can attack cancer. The primary difference is that TCR takes advantage of the body’s natural system of recognizing antigens with the histocompatibility complex (MHC) while CAR-T Cell therapy genetically engineers the T-cell to express chimeric antigen receptors.
CAR-T cell therapies were first FDA approved for treating lymphoma and leukemia, with approval for multiple myeloma just as recently as March 2021. There are limitations however with using CAR-T cell therapy for solid tumors. Firstly, CAR-T cells are introduced into the blood stream so it is much easier for them to access blood based cancers, whereas they are not as successful at infiltrating tumor tissue. The other issue is antigen heterogeneity. CAR-T cells are engineered for a specific antigen, but not all tumor cells are going to express that antigen, and levels of expression may vary. Finally, solid tumors can be infiltrated by cells that support tumor growth and suppress the immune response.
Another limitation of CAR-T cell therapy is that it must be done using the patient’s own T-cells, what is known as autologous CAR-T cell therapy. However, because of other treatments that the patient may have gone through, their t-cells may be depleted. Research is being done into allogenic CAR-T cell therapy, which would be the same basic process, except using a healthy donor’s T-cells.
Natural Killer (NK) Cell Therapy: As previously mentioned, one of the limitations with T-cells is that they target a specific antigen. This is why researchers are also beginning to explore using natural killer cells in a similar type of therapy. Natural killer cells are another type of immune cell, but unlike T-cells they can go after a wider range of threats, as opposed to a specific threat. In addition, early research indicates they may not have some of the side effects that CAR-T cell therapy can have, such as the transplanted cells attacking the host as a foreign entity or releasing inflammatory signaling molecules. There is also a higher potential for success with allogenic treatment, which would allow donors to be used. Natural killer cells however are by no means perfect. There are still difficulties with infiltration of solid tumors, difficulties in manufacturing enough of them outside the body for reintroduction, and getting them to last once they are in the body.
So, what role does the histotech play in adoptive cell transfer therapies such as CAR-T? Check out the new webinar, recently added to the elearn.nsh.org on-demand library, CAR-T Cell Treatments to learn what you’ll need to know as adoptive cell transfer therapies gain traction in modern cancer treatment.
References:
By: Natalie Paskoski, NSH Communications Specialist
#2021
#IHCandMolecular
#Blog